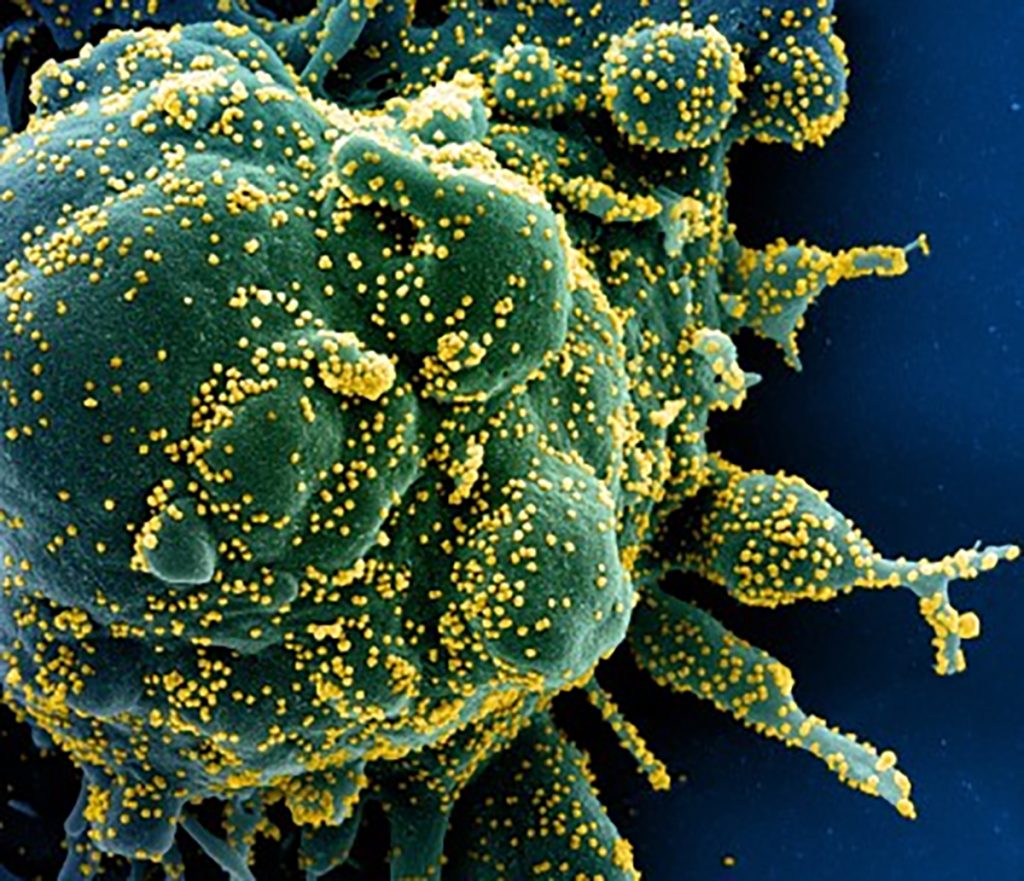
(Newswise) — LA JOLLA, CA—New research from scientists at La Jolla Institute for Immunology (LJI) suggests people who received COVID-19 vaccines and then experienced “breakthrough” infections are especially well armed against future SARS-CoV-2 infections.
By analyzing blood samples from study volunteers, the LJI researchers discovered that people who experienced symptomatic breakthrough infections develop T cells that are better at recognizing and targeting SARS-CoV-2, including the Omicron and Delta variants.
The researchers describe this increased protection as an “immunity wall.”
“The virus evolves, but, importantly, so does the immune system. T cells do not sit idle. Instead, they learn to recognize the parts of the virus that mutate,” says LJI Professor Alessandro Sette, Dr.Biol.Sci., who co-led the Cell Reports Medicine study with LJI Professor Shane Crotty, Ph.D., and LJI Research Assistant Professor Alba Grifoni, Ph.D.
Key findings:
• Study volunteers who experienced symptomatic breakthrough infections developed T cells that recognized multiple targets on the SARS-CoV-2 viral “Spike” and non-Spike epitopes.
• This infection left study volunteers with T cells that were better equipped to recognize mutated regions on new SARS-CoV-2 variants.
• Even asymptomatic breakthrough infections boost T cell responses, though the effect was not as significant.
• Breakthrough infections also led B cells to produce cross-reactive antibodies against SARS-CoV-2. Most of these antibodies targeted the new viral variants and the original vaccine antigens.
• The researchers found no evidence of harmful “T cell exhaustion” in study volunteers who had experienced repeated COVID-19 vaccinations and SARS-CoV-2 infections.
T cells gain fighting power
Many studies have shown that vaccination against SARS-CoV-2, the virus that causes COVID-19, provides people with significant immune protection against severe disease. Several LJI-led studies have shown that this immune protection is long-lasting and can even help protect the body from new viral “variants of concern.”
For the new study, LJI scientists investigated exactly how breakthrough infections affect T cells and B cells. The researchers followed a large group of study volunteers who had been vaccinated against SARS-CoV-2, the virus that causes COVID-19. Over time, many of these volunteers experienced breakthrough infections. The LJI scientists followed up with these volunteers to collect new blood samples post infection.
“With this study volunteer cohort, we were in a unique position to see how the immune system looked before and after a breakthrough infection,” says Grifoni.
Study co-first author and LJI Postdoctoral Researcher Alison Tarke, Ph.D., spearheaded research showing that breakthrough infections prompted T cells to expand their “repertoires.” That meant the cells could recognize multiple features, or antigens, on SARS-CoV-2.
These T cells appeared to develop their broad repertoires due to a combination of vaccination and breakthrough infection. COVID-19 vaccines taught the T cells to recognize a key part of SARS-CoV-2 called the “Spike” protein. Meanwhile, SARS-CoV-2 infection prompted T cells to recognize Spike, as well as several other viral proteins.
Breakthrough infection had left these study volunteers with T cells that could recognize and target SARS-CoV-2, even if part of it was mutated.
More layers of protection
Breakthrough Omicron and Delta variant infections also prompted B cells to produce more diverse antibodies. These antibodies could target epitopes that the vaccine and the infecting SARS-CoV-2 variant had in common.
In fact, most of these new antibodies were good at attacking epitopes that the vaccine and the variants had in common. “New B cell responses that are only specific to the infecting variant, but not the vaccine, are very rare,” says study co-first author and LJI Instructor Parham Ramezani-Rad, Ph.D.
The researchers uncovered another interesting trend in people with breakthrough infections. COVID-19 vaccines tend to be given in the upper arm, which means anti-SARS-CoV-2 immune cells develop far away from the upper respiratory system. SARS-CoV-2 tends to infect the upper respiratory tract first, which means there can be a delay getting the right immune cells to the scene of infection. “A breakthrough infection has the potential of adding a layer of protection on top of a vaccine,” says Grifoni.
What about asymptomatic infections?
As they worked, the scientists also found markers of previous SARS-CoV-2 infection in about 30 percent of study volunteers who had never shown COVID-19 symptoms. These volunteers appeared to have contracted asymptomatic cases of COVID-19 at some point earlier in the pandemic.
“Our study suggests most people who never thought they got a breakthrough infection actually did,” says Grifoni. “The majority of the population appears to be affected by a combination of vaccination and one or more breakthrough infections.”
No evidence of T cell exhaustion
The new study also addresses concerns that repeated infection or COVID-19 vaccine might lead to a phenomenon called T cell exhaustion, where T cells lose their ability to target a pathogen.
The researchers discovered that breakthrough infections prompted T cells to produce more types of cytokines, signaling molecules that help fight infection. Before a breakthrough infection, T cells might produce one or two types of cytokines, Grifoni explains.
“After the breakthrough infection, the same cells produce multiple types of cytokines, making them more efficacious,” says Grifoni. “Not only are our T cells not exhausted, but they are actually improving their capabilities.”
The “immunity wall” does seem to have limits. Following an asymptomatic breakthrough infection, T cell abilities appeared to plateau in response to a subsequent symptomatic infection. B cells continued to produce neutralizing antibodies following subsequent breakthrough infections, but the researchers didn’t see the same big “boost” to neutralizing antibody levels.
So should people continue to get SARS-CoV-2 booster vaccines? The LJI scientists point out that SARS-CoV-2 continues to evolve, and COVID-19 can still cause serious illness in immunocompromised people. Their advice is to follow all current CDC guidelines on who should receive booster vaccines.
Discovery may guide vaccine efforts
This research is also an important step toward the development of new vaccines against future SARS-CoV-2 variants and many other viruses with pandemic potential.
Ramezani-Rad says the study helps answer important questions about how breakthrough infections alter antibody responses. Going forward, he is curious how future SARS-CoV-2 variants—or new vaccine designs—might further tweak the immune system.
“Studies of local B cell responses in the upper airway—where the infection occurs—will also be informative on how B cells responses are induced, particularly after breakthrough infection,” says Ramezani-Rad.
Sette and Grifoni are focused on how to train T cells to recognize many types of coronaviruses at once. Their research is critical for developing a “pan-coronavirus” vaccine.
In a 2023 study, their laboratories worked with scientists at the University of Genoa to show that some T cells can recognize multiple coronaviruses at once. This new study shows them how breakthrough infections can shape T cell responses to fight novel SARS-CoV-2 variants.
“We’re very interested to see if this phenomenon could be exploited in general to prepare against other potential pandemic threats,” says Sette. “This is a step in a journey to help us protect against viral infections and potential pandemics.”
Additional authors of the study, “SARS-CoV-2 breakthrough infections enhance T cell response magnitude, breadth, and epitope repertoire,” include Tertuliano Alves Pereira Neto, Yeji Lee, Vanessa Silva-Moraes, Benjamin Goodwin, Nathaniel Bloom, Leila Siddiqui, Liliana Avalos, April Frazier, Zeli Zhang, Ricardo da Silva Antunes, and Jennifer Dan.
This study was supported by the National Institutes of Health (NIH; T32AI125179), the NIH National Institute of Allergy and Infectious Diseases (75N93021C00016, 75N9301900065, and AI142742.)